QEII Hospital’s Intensive Care Unit (ICU) Education Team has proven small steps equal big leaps for patient outcomes, after the team successfully implemented a new blood glucose management model at the unit and claimed the 2024 International Nurses Day (IND) Improvement of the Year Award for their efforts.
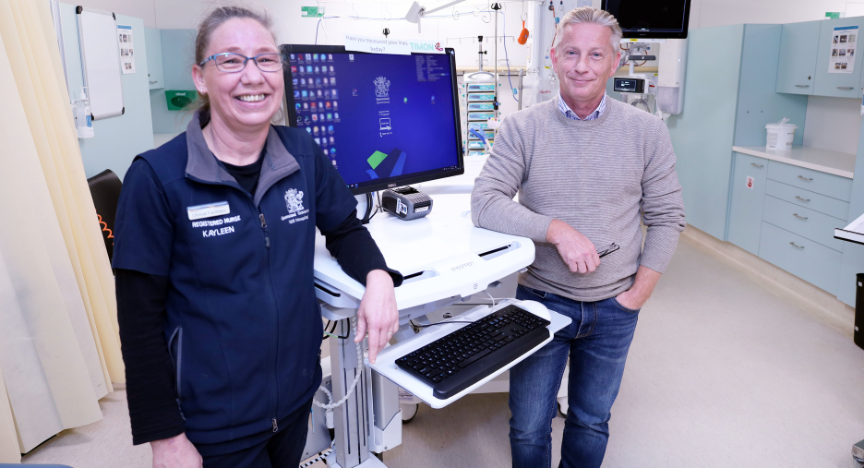
The Insulin Infusion in the Intensive Care Unit initiative is a nurse-led quality improvement passion project developed over the last three years by Clinical Facilitator Kayleen Wheeler with support from ICU Director Dr David Stewart.
Passionate about enhancing care for critically ill patients, Kayleen says it was her own inquisitive nature and a well-timed alignment of data that brought the project to fruition.
“We know from the literature that high blood glucose levels can have a significant impact on mortality and morbidity in critically ill patients, including non-diabetic patients,” Kayleen explained.
“I’d been doing a lot of research on this, and it just so happened that Dr Stewart approached me about a high rate of script re-writes in ICU at that time. The traditional approach to managing blood glucose was very standardised and not tailored to individual patients, so we pulled our data together and came up with a more proactive framework.”
From collating research data on improving blood glucose in critically ill patients, to leading consultation and implementing standardised nurse training across the unit, Kayleen had three key goals in mind.
“Between picking up the increase in blood glucose, getting a script written and getting blood glucose levels back into a normal range, the data showed we were taking too long to start that process, with frequent and extreme fluctuations in blood glucose levels.
“Getting blood glucose levels under control within the first couple of hours and maintaining those levels is really important, so our first goal was to reduce the time it takes to start insulin. The second goal was to get those levels within a normal range in the first four hours.
“Once we got patients into range, we found levels were still fluctuating up and down, pushing them back out of the normal range. To prevent those fluctuations and maintain a normal range was our third goal,” she explained.
It’s the project’s proactive approach to blood glucose monitoring and its tailored application to the unique challenges of the ICU environment that stood it apart from traditional methods.
“Rather than waiting for blood sugar to get out control and going back to the doctor to change scripts, we can use our in-depth clinical knowledge to make a clinical decision that will proactively maintain blood glucose control.”
Cited for improving the quality of ICU care and for empowering more nurses to work to the top of their scope, the award underscores the importance of investing in the multidisciplinary team for best patient outcomes.
“From a nursing perspective, it’s about elevating our nurses to work more autonomously and grow their own skills rather than always relying on doctors,” explained Kayleen.
“We are clinicians in our own right, and we have the capability to make decisions and work to the top of our scope.”
Taking her inquisitive eye to new research ideas, Kayleen looks forward to investing in more forward-thinking nursing education initiatives at the unit.
“I like when I see staff develop the confidence in their knowledge and understanding to be proactive and assertive when necessary, to embrace and advocate for best practice for their patient.”
“I’d also like to thank my line manager Sarah Barrett, who affords me the autonomy and freedom to pursue my ideas and provides great mentorship and support.”
Congratulations on this fantastic initiative and the well-deserved recognition, team.